If you’ve been living with constant muscle aches, stiffness, and exhaustion, you might have searched your symptoms online and stumbled across the word “inomyalgia.” It appears on health blogs, forums, and a few small websites, usually described as a form of chronic muscle pain that doesn’t show up clearly on tests.
But what exactly is inomyalgia? Is it a new disease, another name for fibromyalgia, or just a descriptive label people use when they’re struggling to explain their pain?
This article takes a detailed look at what the term inomyalgia usually means online, how it overlaps with other chronic pain conditions, why it’s important to treat it cautiously, and what practical, evidence-based steps may actually help with long-term muscle pain.
Important note: Inomyalgia is not currently recognized as an official medical diagnosis by major health organizations. The information below is educational only and not a substitute for professional medical advice. Always talk to a qualified healthcare provider about your symptoms.
What Does “Inomyalgia” Mean?
To understand the term, it helps to break it down:
- “Ino” – often interpreted as relating to muscle fibers or tissue
- “Myalgia” – medical term for muscle pain
So, inomyalgia is commonly presented as meaning “muscle-fiber pain” or “chronic muscle pain.”
On blogs and general health websites, inomyalgia is usually described as:
- A chronic condition involving long-lasting muscle pain
- Often non-inflammatory (blood tests may look normal)
- Linked to how the nervous system processes pain
- Similar to or overlapping with fibromyalgia, but sometimes portrayed as a more “muscle-focused” version
However, unlike fibromyalgia, inomyalgia does not appear in major diagnostic manuals or guidelines. There are no large clinical trials, no official criteria, and no widely accepted definition outside of online discussions and a few niche websites.
Because of that, it’s better to think of inomyalgia as a descriptive label that people use for a certain pattern of chronic muscle pain, rather than a firmly established disease with clear boundaries.
How Inomyalgia Is Described Online
If you scan through blogs and posts that mention inomyalgia, you’ll notice a few recurring themes:
- Chronic muscle pain is the central feature
- Symptoms may be localized (e.g., neck, shoulders, lower back) or widespread
- There’s often no obvious injury or structural damage on scans
- Many writers link it to fibromyalgia, chronic fatigue, or central sensitization
Some websites call inomyalgia an “emerging condition” or a “subtype” of chronic pain; others simply use it as a more specific name for ongoing muscle pain that doesn’t fit neatly into other diagnoses.
In practice, many people using the word inomyalgia are experiencing fibromyalgia-like symptoms, but they either:
- Don’t feel that the fibromyalgia label fits them, or
- Haven’t received a formal diagnosis, or
- Prefer a term that emphasizes muscles rather than “everywhere pain”
Common Symptoms Attributed to Inomyalgia
Although there are no official criteria, the symptoms described online under the label “inomyalgia” tend to fall into several categories.
1. Pain and Physical Discomfort
- Persistent muscle pain – aching, burning, or soreness
- Pain that may be:
- Localized in a few muscle groups (e.g., neck, shoulders, lower back, hips), or
- More spread out across the body
- Stiffness, especially after waking or sitting for a long time
- Pain that fluctuates – some days better, some days worse
2. Fatigue and Low Energy
Many descriptions include significant fatigue, such as:
- Feeling tired even after a full night’s sleep
- “Heavy” limbs or low stamina
- Needing more rest than others after normal activities
3. Sleep Disturbances
Common sleep-related issues include:
- Trouble falling asleep or staying asleep
- Waking up feeling unrefreshed, as if you haven’t really rested
- Night-time pain that disrupts sleep
4. Cognitive and Emotional Symptoms
Some people who use the inomyalgia label also report:
- “Brain fog” – difficulty focusing, forgetfulness, slowed thinking
- Irritability, anxiety, or low mood after dealing with pain for a long time
- Feeling “not like myself,” mentally and emotionally
5. Sensitivity and Flare-ups
It’s also common to read about:
- Increased sensitivity to touch, temperature, or pressure
- Pain flare-ups triggered by stress, lack of sleep, over-exertion, or even changes in weather
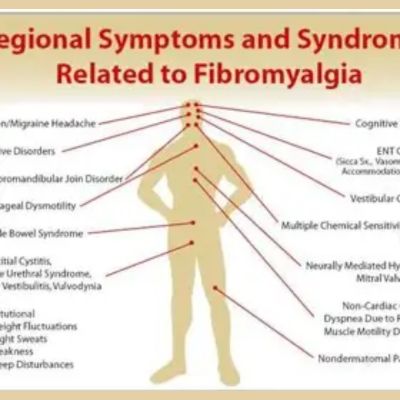
These symptoms overlap strongly with fibromyalgia, chronic widespread pain, and other chronic pain syndromes. This is one reason many experts view inomyalgia as simply part of the chronic pain spectrum, rather than a distinct new disease.
Possible Causes and Mechanisms (Based on Current Understanding of Chronic Pain)
Because inomyalgia isn’t well-studied, most of the explanations you’ll see are educated guesses borrowed from research on fibromyalgia and other chronic pain conditions.
A few key ideas:
1. Central Sensitization
One widely accepted concept in chronic pain science is central sensitization – changes in the brain and spinal cord that make the nervous system more sensitive to pain signals.
In this model:
- The nervous system becomes “wound up” and over-reactive
- Normal sensations (like light pressure or minor strain) can be perceived as painful
- The volume knob on pain is turned up, even though tissues may look normal on scans
Many blogs that mention inomyalgia describe it as central sensitization focused on muscle pain.
2. Stress, Sleep, and Lifestyle Factors
Chronic muscle pain is usually multifactorial, meaning there’s no single cause. Contributing factors may include:
- Long-term stress and emotional pressure
- Poor sleep or disrupted sleep cycles
- Sedentary lifestyle and lack of movement
- Repetitive strain or poor posture over many years
- Past injuries (even if they’ve “healed”) that changed movement patterns
These factors can interact with each other and with the nervous system, creating a cycle where pain → stress → poor sleep → more pain.
3. Biological Susceptibility
Some people may be more vulnerable due to:
- Genetic tendencies toward pain sensitivity or mood disorders
- Hormonal changes (e.g., cortisol, serotonin) that influence pain and mood
- Nutritional deficiencies (such as low vitamin D or B12), although these are usually contributing factors rather than sole causes
Again, this is all general chronic pain science, not specific research on “inomyalgia” as a unique condition. That’s why medical professionals are cautious about adopting the term.
Inomyalgia and Fibromyalgia: How Are They Related?
This is the big question many readers have:
“Is inomyalgia the same as fibromyalgia?”
Right now, the most honest answer is:
- Fibromyalgia is a well-recognized clinical syndrome with established criteria.
- Inomyalgia is an unofficial term used mostly online to describe chronic muscle pain that often looks very similar to fibromyalgia.
Fibromyalgia (Brief Overview)
Fibromyalgia typically involves:
- Widespread pain on both sides of the body and above/below the waist
- Symptoms lasting at least three months
- Significant fatigue, unrefreshing sleep, and cognitive difficulties
- Diagnosis based on symptom patterns and ruling out other diseases
It is recognized by major health bodies and appears in clinical guidelines.
Inomyalgia (As Described Online)
- Emphasizes muscle pain, sometimes more localized
- Often overlaps with fatigue, sleep issues, and brain fog
- Has no standardized diagnostic criteria
- Is not officially recognized as a separate disease
Some blogs try to distinguish inomyalgia as:
- More localized muscle pain versus the widespread pain of fibromyalgia
- More muscle-dominant (pain and stiffness) with slightly fewer systemic symptoms
However, without research and formal definitions, these differences are largely theoretical. In real life, many people’s symptoms blur these lines.
Diagnosis: Why Self-Labeling Can Be Risky
Because the word “inomyalgia” is not an official diagnosis, doctors are unlikely to write it in your medical chart. When you visit a healthcare professional, they’re more likely to evaluate you for:
- Fibromyalgia
- Chronic widespread pain
- Myofascial pain syndrome
- Arthritis, connective tissue diseases
- Endocrine or metabolic issues (like thyroid disease)
- Neurological or other underlying conditions
A proper diagnosis process may involve:
- A detailed medical history and symptom review
- Physical examination, including joints and muscles
- Blood tests or imaging to rule out other causes
This is crucial, because symptoms such as fatigue, pain, and sleep problems are not specific – they can be caused by many different conditions, some of which require very different treatments.
Relying solely on an internet label like “inomyalgia” and skipping medical evaluation can mean:
- Delayed diagnosis of treatable conditions
- Using strategies that aren’t appropriate for your situation
- Increased anxiety from guessing or mislabeling your symptoms
So, while you may use the term inomyalgia to describe your experience, it should not replace a professional assessment.
Management and Self-Care: What Actually Helps?
Even though inomyalgia itself isn’t a formal diagnosis, many of the strategies suggested on blogs are adapted from evidence-based approaches for chronic pain and fibromyalgia.
Here are some commonly recommended directions you can discuss with your healthcare provider:
1. Work With a Healthcare Professional
Start with:
- Your primary care doctor, who can rule out urgent issues and order initial tests
- If needed, a rheumatologist, neurologist, or pain specialist
Together, you might consider:
- Non-opioid pain relievers where appropriate
- Medications that help modulate pain and improve sleep (e.g., certain antidepressants or anti-seizure drugs, prescribed and monitored by a doctor)
- Treatment of coexisting issues like depression, anxiety, or sleep disorders
Never start, stop, or change medication without professional guidance.
2. Gentle, Regular Movement
Movement is one of the most powerful tools in chronic muscle pain, even when it feels counterintuitive.
Helpful options can include:
- Walking at an easy pace, gradually increasing time
- Stretching to improve flexibility and reduce stiffness
- Low-impact exercises such as swimming, water aerobics, or cycling
- Yoga or Pilates, modified to your level
Key principles:
- Start small, even 5–10 minutes
- Increase slowly to avoid flare-ups
- Focus on consistency, not intensity
A physiotherapist or physical therapist experienced in chronic pain can design a personalized program that respects your limits and helps you build resilience over time.
3. Sleep Hygiene
Because poor sleep worsens pain (and pain worsens sleep), improving sleep habits can make a real difference:
- Go to bed and wake up at consistent times
- Reduce screen time and bright light in the hour before bed
- Create a calming pre-sleep routine (warm shower, light reading, relaxation exercises)
- Limit heavy meals, caffeine, and nicotine in the evening
If insomnia or sleep apnea is suspected, talk to your doctor about further evaluation.
4. Stress Management and Mental Health
Living with chronic pain is emotionally draining. Anxiety, fear, and frustration can all increase pain sensitivity.
Helpful tools may include:
- Cognitive-behavioural therapy (CBT) or other counselling
- Relaxation techniques: deep breathing, progressive muscle relaxation, guided imagery
- Mindfulness or meditation practices
- Support groups (online or in person) for people with chronic pain
Taking your emotional health seriously is not a sign of weakness – it’s a key part of treating the whole person, not just the pain.
5. Lifestyle and Nutrition
Although no specific “inomyalgia diet” exists, general healthy habits can support your body:
- A balanced diet rich in whole foods, fruits, vegetables, lean protein, and healthy fats
- Adequate hydration
- Discussing vitamin D, B12, or other supplements with your doctor if you suspect deficiencies
- Avoiding crash diets and extreme restrictions that might worsen fatigue
When Should You Seek Medical Help Urgently?

Chronic muscle pain with stable, long-term symptoms is different from sudden or rapidly worsening pain. Seek urgent medical attention if you experience:
- New, severe, or rapidly progressing pain
- Pain accompanied by fever, unexplained weight loss, or night sweats
- Weakness, loss of coordination, or trouble walking
- Chest pain, shortness of breath, or other emergency symptoms
- Changes in bladder or bowel control
- Any symptom that feels alarming or very different from your usual pattern
Even if you believe you have “inomyalgia,” new or severe symptoms should never be ignored.
Living With Inomyalgia-Type Pain: A Realistic Perspective
Whether you call it inomyalgia, chronic muscle pain, or fibromyalgia-like symptoms, the experience is real and life-changing. It can affect your work, relationships, mood, and identity.
A realistic approach includes:
- Accepting that there may not be a single, simple label
- Focusing on what you can control: habits, pacing, sleep, stress, movement
- Building a care team you trust (doctors, physio, therapist, supportive family/friends)
- Celebrating small improvements and not measuring yourself against your “old” self every day
In the end, a word like inomyalgia can sometimes provide comfort – it lets people say, “This is what I’m going through.” But the label is less important than finding practical ways to reduce pain, protect your function, and improve your quality of life.
Final Thoughts – and a Note from Buz Vista
The term inomyalgia is, for now, more of an online concept than a recognized medical diagnosis. It reflects a growing awareness that chronic muscle pain, even when tests look “normal,” is real and deserves attention, compassion, and science-based care.
If your symptoms sound similar, the best next step is not to self-diagnose, but to partner with a healthcare professional, share your full story, and explore the range of chronic pain management options that exist today.
At Buz Vista, our goal is to take confusing, sometimes vague health terms like inomyalgia and unpack them in a clear, honest way—connecting everyday experience with what we actually know from research and clinical practice. We hope this deep dive has given you language for what you’re feeling, a more grounded understanding of what might be happening in your body, and encouragement to seek the support you deserve.
If you’d like more guides like this—on chronic pain, fatigue, and navigating modern health information—stay tuned to Buz Vista for evidence-informed, reader-friendly explanations you can actually use in real life.
FAQS ABOUT INOMYLGIA
1. What is inomyalgia?
Inomyalgia is an unofficial term used mostly on blogs and health websites to describe chronic muscle pain that may be widespread or localized. It often overlaps with symptoms seen in fibromyalgia, such as fatigue, stiffness, sleep issues, and “brain fog,” but it is not yet recognized as an official medical diagnosis.
2. Is inomyalgia the same as fibromyalgia?
Not exactly, but they’re closely related in how people describe them.
- Fibromyalgia is a recognized condition with established diagnostic criteria and guidelines.
- Inomyalgia is more of an informal label for persistent muscle pain, usually with fibromyalgia-like features.
Many people who think they have inomyalgia may actually meet criteria for fibromyalgia or another chronic pain condition.
3. Is inomyalgia a real disease?
The pain is real, but the term “inomyalgia” is not an officially accepted medical diagnosis at this time. Doctors are more likely to diagnose related conditions such as fibromyalgia, chronic widespread pain, or myofascial pain syndrome. Inomyalgia is mainly a descriptive word used online to talk about a certain pattern of chronic muscle pain.
4. What are the most common symptoms of inomyalgia?
People who use the term inomyalgia often report:
- Ongoing muscle pain and tenderness
- Stiffness, especially after rest or in the morning
- Fatigue and low energy
- Poor or unrefreshing sleep
- Difficulty concentrating or “brain fog”
- Occasional mood changes, irritability, or low mood
Symptoms can vary in intensity from day to day and may flare up with stress, over-exertion, or lack of sleep.
5. What causes inomyalgia?
There is no single proven cause because inomyalgia itself hasn’t been formally researched as a separate condition. Most explanations come from what we know about chronic pain in general and fibromyalgia, including:
- Changes in how the nervous system processes pain (central sensitization)
- Long-term stress and emotional strain
- Poor sleep or sleep disorders
- Reduced physical activity or deconditioning
- Past injuries, poor posture, or repetitive strain
- Possible genetic and hormonal influences
For any individual, several of these factors may be involved at the same time.
6. How is inomyalgia diagnosed?
There is currently no official test or criteria specifically for inomyalgia. A doctor will not usually diagnose “inomyalgia” by name. Instead, they will:
- Take a detailed medical history and symptom description
- Perform a physical exam, including muscles and joints
- Order tests if needed to rule out other conditions (e.g., arthritis, thyroid disease, infections, autoimmune disorders)
In many cases, people who think they have inomyalgia may end up with a diagnosis such as fibromyalgia, myofascial pain, or chronic widespread pain.
7. Can I self-diagnose inomyalgia?
You can certainly recognize patterns in your own symptoms, but self-diagnosing any condition based solely on internet information is risky. Symptoms like pain and fatigue are nonspecific and can be caused by many different problems. It’s important to see a healthcare professional to:
- Exclude serious or treatable conditions
- Get appropriate tests, advice, and treatment options
- Avoid unnecessary fear or misunderstanding about your symptoms
Use terms like “inomyalgia” only as a conversation starter, not as a final answer.
8. How is inomyalgia treated?
Since inomyalgia isn’t an official diagnosis, treatment usually follows chronic pain and fibromyalgia management principles, for example:
- Working with a doctor on safe, non-opioid pain relief options
- Considering certain medications that help modulate pain and improve sleep (as appropriate)
- Gentle, regular exercise such as walking, stretching, yoga, or swimming
- Physiotherapy for posture, flexibility, and strength
- Sleep hygiene: consistent routine, limiting screens, calming bedtime habits
- Stress management: CBT, counselling, relaxation techniques, mindfulness
- Healthy lifestyle habits and a balanced diet
Always discuss any treatment or supplement with your doctor first.
9. Can inomyalgia be cured?
Most chronic pain conditions, including those described as inomyalgia, don’t have a quick “cure.” However, many people do improve significantly with the right combination of:
- Medical treatment
- Movement and physical therapy
- Better sleep and stress management
- Emotional and social support
The goal is often management and quality of life, not perfection—but meaningful progress is possible.
10. Is inomyalgia dangerous or life-threatening?
Inomyalgia-type muscle pain is usually not life-threatening by itself, but it can be very disruptive and emotionally draining. The real concern is that pain and fatigue might be caused by an underlying condition that needs attention. That’s why a proper medical evaluation is essential—especially if symptoms are new, severe, or rapidly changing.
11. Should I tell my doctor I think I have inomyalgia?
Yes, you can. You might say something like:
“I’ve read online about inomyalgia and chronic muscle pain. These descriptions sound similar to what I’m experiencing. Can we talk about what might be causing my symptoms?”
Your doctor may not use the word “inomyalgia,” but they can help translate your symptoms into a clinical picture, suggest tests, and plan appropriate treatment options.
12. How can I cope emotionally with inomyalgia-type pain?
Chronic muscle pain affects more than just your body. Helpful coping strategies include:
- Talking honestly with family and friends about what you’re going through
- Joining support groups (online or offline) for people with chronic pain
- Working with a therapist or counsellor, especially if you feel depressed, anxious, or overwhelmed
- Setting realistic goals and pacing your activities to avoid boom-and-bust cycles
- Celebrating small wins and progress, not just focusing on what you can’t do
Remember, you’re not weak for needing help—you’re human, and chronic pain is a heavy load for anyone to carry alone.